What I Learned at APAC 2025: The Research That Changes How We Support Autistic Children
Nov 24, 2025
Three days of cutting-edge autism research, translated for your practice
I've recently returned from the Asia Pacific Autism Conference in Perth, and my notebook is filled with research that I know will transform how we work with autistic children.
I spent three days (and several thousand dollars in registration, flights, and accommodation) attending keynotes, concurrent sessions, and networking with researchers from around the globe. I took detailed notes, photographed slides, and asked questions so I could bring this knowledge directly to you.
Because this is what I love doing: taking all the new knowledge and breaking it down into content that OTs can easily digest and use in practice. #WeDoTheResearchSoYouDontHaveTo
What I learned at APAC 2025 reinforces something we need to talk about more openly: impairment in autism isn't inherent. It's created by our failure to include autistic individuals in activities, environments, and daily life in ways that honour how they experience the world.
When we restrict access and assume limited capabilities, we create the very limitations we then measure. But when we create inclusive spaces, adapt classroom curricula, and open extracurricular activities to all learning styles, we open an entire world of possibilities.

Here's what the research is telling us:
Day 1: Meeting People Where They Are
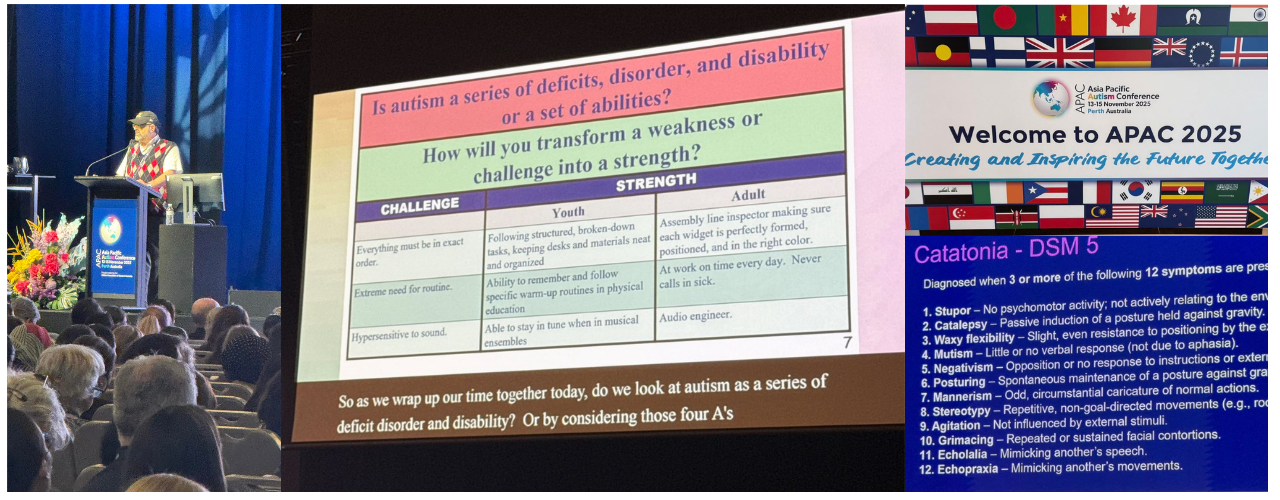
Dr Stephen Shore: When Accommodation Enables Participation
Dr Stephen Shore, an autistic individual, advocate, and music teacher, opened the conference by sharing his childhood experience of joining the music club at school. Initially, he joined to take apart and reassemble all the instruments (a sensory and special interest that made perfect sense to him). When he heard that learning 15 instruments would be beneficial, he learned all 15.
He applied this same approach to bicycles as a teenager, eventually working in a bicycle repair shop. His interests weren't deficits. They were pathways to skill development and employment when someone recognised their value.
His message centred on the Four A's of autism: Awareness, Acceptance, Appreciation, and Action. He challenged all of us to consider: what action are we taking to broaden ourselves across all four areas?
His core message: "Developing a trusting relationship and meeting them where they are at. Looking for interests and strengths as soon as possible in the journey and focusing on supporting self-advocacy in all iterations."
Here's what struck me most: Dr Shore wears his cap during presentations to block out bright lights, which he describes as being like staring into a strobe light. Without this simple accommodation, he would be 'disabled' from presenting. With it, he shares his expertise with hundreds of professionals.
This is the point. The impairment isn't in him. The impairment is in environments that don't consider sensory needs.
Autism and Catatonia: What We're Missing
Prof Matthew Siegel presented research on autism and catatonia that completely challenged my preconceptions. Like many professionals, I'd associated catatonia with an almost comatose state. The research shows it can present as the complete opposite.
Up to 10.5% of autistic individuals may experience catatonia, according to recent studies. The DSM-5 defines catatonia as a motor and behavioural syndrome characterised by marked changes in movement (either very little or excessive), mutism and negativism, posturing and waxy flexibility, and echolalia and echopraxia.
This is frequently missed in clinical practice because of symptom overlap with autism itself. We need to be more alert to these presentations, particularly when we see sudden regression or marked changes in a child's movement patterns.
Neurodivergent-Affirming Practice: The New Standard
The concurrent sessions presented a wonderful challenge: choosing between at least ten options per 20-minute slot. What stood out across every presentation I attended was that neurodivergent-affirming dialogue and practice wasn't a 'nice to have'. It was the foundational paradigm.
Hot topics included caregiver stress, autistic social anxiety, and "intolerance of uncertainty". One presentation particularly moved me: a Singaporean mother of a profoundly autistic child developed a new framework for her child's unique communication style, which she terms ALIS (Autistic Language: Instinct and Senses). She's written a book carrying a message of love, patience, and attunement.
This mother didn't wait for the world to accommodate her child. She created the accommodation herself, then shared it so other families could benefit. This is what inclusion looks like in practice.
Day 2: Trauma, Environment, and What Creates "Impairment"
Autism, Trauma, and PTSD: Why Our Diagnostic Criteria Are Failing Autistic Individuals
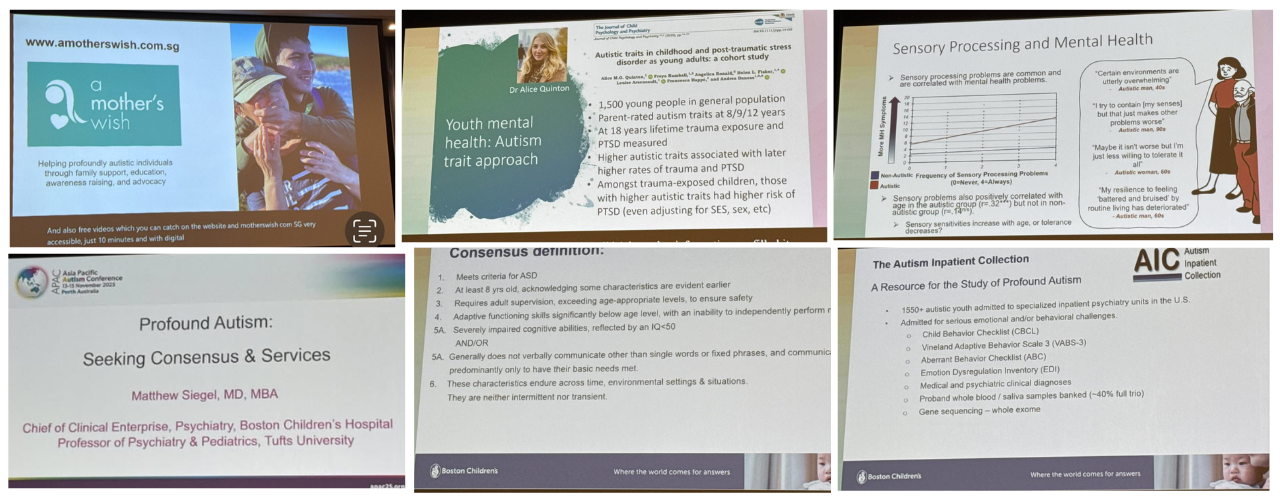
Prof Francesca Happé presented research that should change how we think about trauma assessment in autistic clients.
In their research, trauma that didn't meet DSM-5 criteria but where the person presented with PTSD symptoms occurred in 86% of autistic males and 53% of autistic females studied.
Think about that for a moment. The vast majority of autistic individuals in this study experienced trauma and PTSD symptoms, but their experiences didn't 'count' according to current diagnostic criteria.
Prof Happé's perspective: "It doesn't matter what happened, if you found it traumatic and have the symptoms of PTSD."
If an autistic cognitive style is more detail-focused, paired with heightened sensory experiences and an avoidant coping style, these factors contribute to a higher likelihood of PTSD following events they perceive as traumatic.
The research also found that more autistic symptoms correlated with higher PTSD likelihood, more sensory symptoms were associated with more mental health challenges, and higher levels of masking correlated with increased PTSD risk.
Here's what this means for practice: when we force autistic children to mask, to suppress their sensory needs, to participate in overwhelming environments without accommodation, we're not helping them adapt. We're creating trauma.
The impairment isn't in the child. It's in our failure to create safe, sensory-friendly, inclusive environments where they can participate authentically.
Profound Autism: Redefining Support Needs
Prof Matthew Siegel returned to present research from a massive collaborative project that included medical professionals, lived-experience individuals, and caregivers to propose a new definition of profound autism.
Using this refined definition, they explored their database of over 1,550 autistic individuals and found that 72% would meet criteria for profound autism, versus previous literature estimates of approximately 25%.
This significant difference matters for how we conceptualise support needs, allocate resources, and design services. It also highlights how our previous definitions may have underestimated the support needs across the spectrum.
Sensory Realities: Creating Inclusive Environments
Dr Stephen Shore's second presentation brought his lived experience of significant sensory challenges into sharp focus. He described how sensory overwhelm becomes manageable when certain conditions are met:
Information about the environment beforehand
A degree of control over the environment
The ability to say "stop" or remove himself
Access to his regulatory toolbox
Multiple presenters with lived experience and researchers made this point clear: if the world were more sensory-friendly, the 'disabling' aspects of sensory challenges would be less pronounced and people could live potentially higher quality lives.
Our modern society still doesn't recognise or provide adequate practical, environmental support for sensory individuals. We design classrooms with fluorescent lighting that causes pain. We create open-plan offices with constant auditory bombardment. We schedule back-to-back activities with no regulation breaks. Then we measure the child's 'impairment' in these hostile environments.
What if we designed differently? What if we created inclusive spaces from the start?
Dr Shore also reminded us about language: reframe "self-stimulatory behaviours" as "self-regulatory behaviours." The language we use shapes how we see the child and how we design support.
Gestalt Language Processing: Honouring Different Communication Pathways
Speech-language pathologists from the Autism Association of Western Australia presented on Gestalt Language Processing, offering a framework that honours how some children naturally acquire and use language.
When a child seems rhythmically and musically inclined, uses the same style and intonation each time (echolalia/scripts), and ties these to emotions or experiences as 'chunks' of words, we're likely seeing gestalt language processing.
For example, a child who falls off their bike might say "Are you okay?" because this is the language chunk they've heard when experiencing pain or discomfort. They're not being inappropriate. They're communicating their internal experience using the language tools they have.
When we understand this framework, we can support communication development in ways that honour the child's natural learning style rather than trying to force them into a different pathway. This is inclusion in communication support.
Day 3: The Research That Changes Everything
I could only attend the two keynotes before my flight, but these presentations were the most impactful of the entire conference.
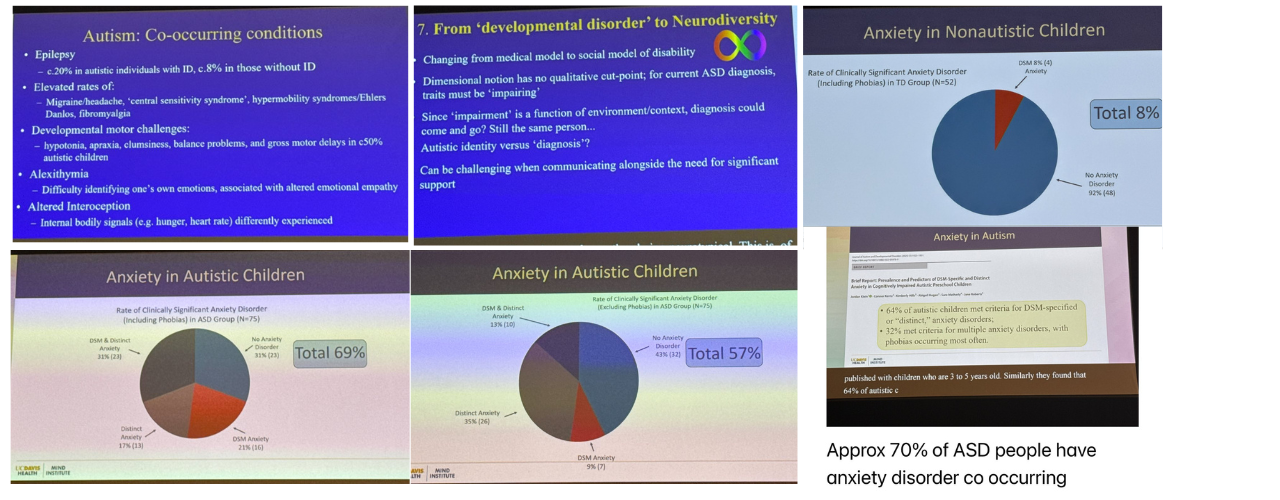
Autism and Anxiety: Beyond DSM-5 Criteria
Prof David Amaral from the USA presented work highlighting the danger of relying solely on DSM-5 criteria to diagnose anxiety in autistic individuals. Their studies showed we'll miss many with distinct anxiety presentations if we stick rigidly to these criteria.
Children with intellectual disability and IQ below 70 presented with more phobias than those with IQ above 70. As a neuroscientist, Prof Amaral established the MIND Institute to continue this work, notably including people with lived experience and affirming methods of data collection in his research approach.
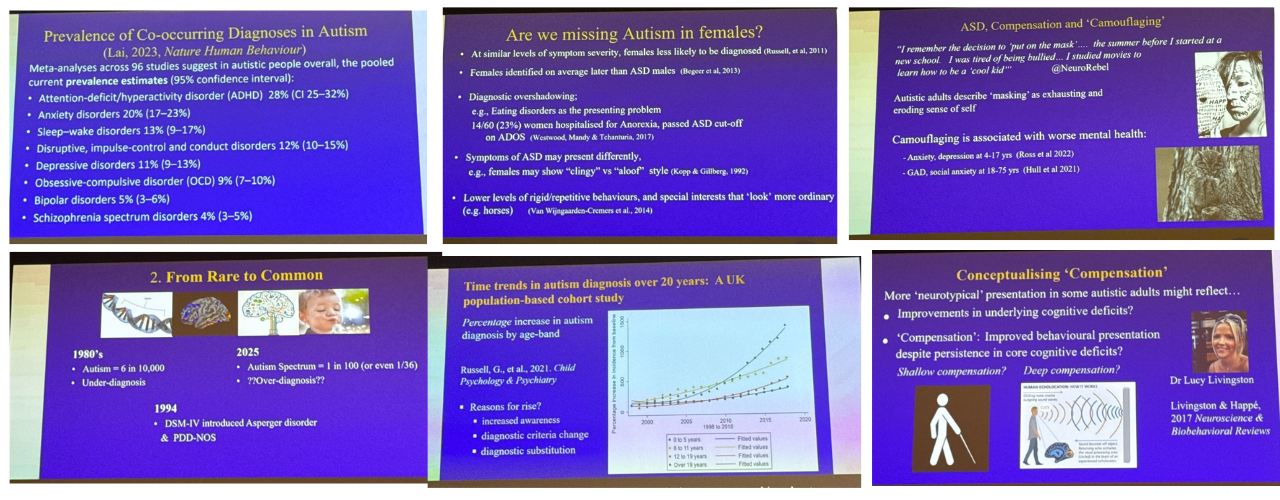
30 Years of Autism Research: What Prof Happé Taught Us About "Impairment"
Prof Francesca Happé's closing presentation synthesised three decades of autism research. What she shared fundamentally challenges how we think about autism diagnosis and support.
How Diagnostic Criteria Have Evolved
The apparent rapid rise in autism diagnosis started after DSM-4 was released in 1994, which included Asperger's and PDD-NOS categories. Prior to this, DSM-3 included intellectual disability as a defining factor. This shift saw a rapid increase in late diagnosis of teenagers, adults, and women and girls.
Why We're Still Missing Women and Girls
Women often present with co-occurring conditions (anorexia nervosa, anxiety disorders) that prevent diagnosticians from looking further. Women and girls present differently: they may be clingy rather than aloof, or eager to express special interests in horses or soft toys, which appears more socially acceptable than mechanical or mathematical interests.
Consider this: boys lining up cars is a red flag, but girls lining up teddies might appear to be playing teacher or decorating their beds. We miss the pattern because we're looking for it to present in boy-typical ways.
The research showed that more masking correlates with lower quality of life (possibly due to exhaustion), higher IQ relates to late diagnosis, and higher masking relates to late diagnosis.
When we fail to diagnose, we fail to provide accommodations and support. We force these girls and women to navigate a world that wasn't designed for them, without the understanding or tools they need. We create impairment through exclusion.
The Critical Word: "Impairment" and What It Really Means
This is the most important takeaway from the entire conference.
Prof Happé paid specific focus to the word "impairment" in DSM-5 diagnostic criteria. She explained that if we get it right with environmental accommodations and strategies, and the individual is living a rich quality of life, then the diagnosis can fall away.
People can move in and out of ASD symptom presentations at different points in life, depending on how supportive the environment is. The same is true for ADHD.
Read that again. The impairment isn't fixed. It's environmental.
When we create inclusive classrooms where sensory needs are honoured, when we design curricula that allows for different processing styles, when we open extracurricular activities to all learning approaches, we don't just support autistic children. We remove the barriers that create impairment.
When we restrict access, assume limited capabilities, and design environments that cause sensory pain, we create the very impairments we then measure and document. We restrict their ability to develop beyond what we assume their capabilities are.
But when we create inclusive spaces, when we adapt and open possibilities, we open an entire world for these children. We see capabilities we never knew existed because we never created the conditions for them to emerge.
This raises the profound question Prof Happé left us with: should we be thinking of autism as an identity rather than a diagnosis?
Understanding Heterogeneity: "Autisms" Not Autism
Prof Happé's research on overlapping genetic influences shows huge heterogeneity in autism presentations. She suggests we might need to think about 'autisms' with emphasis on the plural.
Her research supports that yes, you can be "a little bit autistic." This isn't minimising autism. It's recognising that autism exists on a true spectrum with infinite variations in how it presents.
This matters for how we assess, how we support, and how we design inclusive environments that work for the full range of human neurodiversity.
What This Means for Our Practice: Creating Inclusion, Not Managing Impairment
Three days at APAC 2025 gave me language for what many of us know intuitively: we're not treating impairments. We're removing barriers.
This might look like having an in-depth understanding of the child and their environments to support their sensory needs, strategies and accommodations. This might look like parent education or coaching, advocacy and school strategies.
For us as occupational therapists, this is our work. We understand person-environment fit. We know how to analyse activity demands and modify environments. We're trained to see strengths and build from there.
The research presented at APAC 2025 validates what we do when we do it well and consider the whole child within their different environments, tasks, and cultures.
We create the conditions for capacity to emerge.
As Dr Stephen Shore reminded us, it starts with developing trusting relationships and meeting people where they are. Everything else builds from there.
This is why I spent three days and several thousand dollars at this conference. So I could bring you this research, break it down, and translate it into practical application for your work. Because #WeDoTheResearchSoYouDontHaveTo.
You save the time. You save the money. You get the cutting-edge knowledge delivered in digestible, immediately applicable insights.
And together, we create inclusive worlds where every child can thrive.
Join our Facebook OT Community Group to view the posts and images:

For more evidence-based sensory integration training and resources, visit
The SenseUp Approach Course (Comprehensive Sensory Integration and Trauma Informed Training) for monthly research updates, live mentoring calls, and a community of OTs who understand this work. I do the research, so you don't have to!

Kerry Evetts is an occupational therapist with 27+ years of clinical experience and founder of SenseUp Training and SenseUp Therapies on the Gold Coast. She is passionate about bringing OTs back to the science, so families get the expert support they deserve.
Stay connected with news and updates!
Join our mailing list to receive the latest news and updates from our team.
Don't worry, your information will not be shared.
We hate SPAM. We will never sell your information, for any reason.
